By EngenderHealth. Originally posted on EngenderHealth.org.
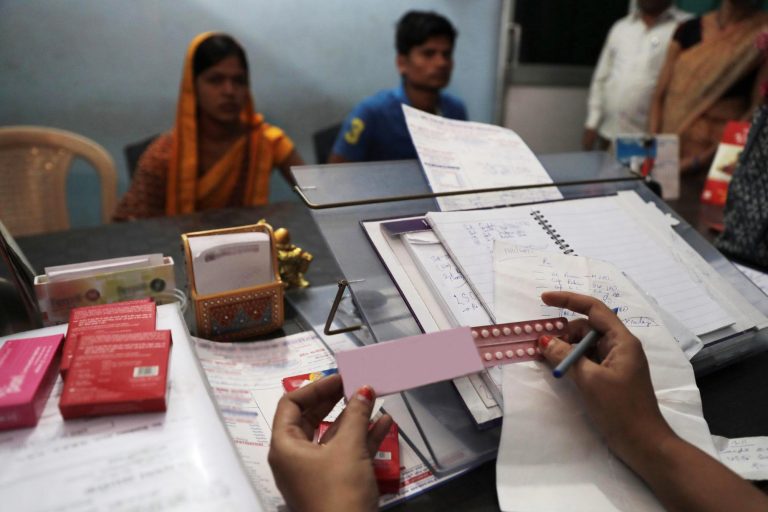
“Many women like me come from a poor family. We use the contraceptives at government hospitals because they are free,” said Geeta*, a 25-year-old mother of two from Gujarat, India.
Not long after the birth of her first child, Geeta chose to have an intrauterine contraceptive device (IUCD) inserted for free at a nearby government hospital so she could determine the timing of her second pregnancy.
However, the COVID-19 pandemic has caused challenges for women like Geeta. On March 24, India implemented a nationwide lockdown considered one of the strictest in the world, which made it cumbersome, and at times impossible, for people to travel to health facilities for contraceptives.
While lockdown measures were recently eased at a national level, there are still hundreds of “containment zones” with restrictions in place, and many people in the country continue to have difficulty accessing contraceptive services and supplies.
Even if someone can get to a health facility or has access to home-based contraceptive services through a community health worker, there is no guarantee that the contraceptive method of their choice will be in stock due to pandemic-related disruptions to contraceptive supply chains.
Devastating impacts
A recent policy brief by the Foundation for Reproductive Health Services India (FRHS India) estimated that, due to the pandemic, millions of Indians will not be able to access their chosen contraceptive methods and that there will be a loss of 709,088 IUCDs, 509,360 doses of contraceptive injections, 20 million cycles of oral contraceptive pills, 827,332 emergency contraceptive pills, 530,737 permanent methods, and 342.11 million condoms.
Even in a best-case scenario in which contraceptive services are at full capacity by July, FRHS India estimates that 24.55 million couples in the country would not have been able to access contraceptives in 2020.
Manisha Wagh, an EngenderHealth-trained senior staff nurse working at a government hospital in Maharashtra, India, believes that “there will be many unwanted pregnancies and abortions” if people cannot obtain the contraceptive methods of their choice and, in turn, forego the use of contraception altogether.
“If clients don’t get the method of their choice, they usually don’t accept other methods,” said Wagh.
In fact, FRHS India estimates that, if the situation does not normalize, the country will experience an additional 1.94 million unintended pregnancies and 1.18 million abortions (including 681,883 unsafe abortions).
Resolving contraceptive stockouts
EngenderHealth’s India team has been working in the states of Karnataka and Maharashtra to strengthen the systems of 144 health facilities—around 40 of which are in lock-downed “containment zones”—to ensure they are fully stocked with available contraceptive methods. To date, the team’s efforts have helped to resolve contraceptive stockouts at roughly 37 of those facilities.
The hospital where Wagh works is one such facility—in April, it experienced stockouts of IUCDs and nonsteroidal oral contraceptive pills.
“Due to the lockdown’s travel restrictions we were not able to go to the district store to get [contraceptive] stocks. We also do not have enough manpower to do this; everyone is busy with screening COVID-19 patients,” said Wagh.
After learning about the hospital’s stockouts from Wagh, EngenderHealth Clinical Trainer Dr. Apurva Akre coordinated with district health officials to find an alternative way to make sure that contraceptive stocks were supplied to the facility.
“I will support facilities to restock [contraceptives] in every way possible,” said Dr. Akre.
Now that the lockdown in India has started to ease up in some areas, Dr. Akre and others on the team are working to ensure that EngenderHealth-supported facilities have the proper systems and coordination mechanisms in place to maintain contraceptive stocks throughout the remainder of the pandemic and upcoming recovery phase.
“We are continuously communicating with our providers and facilities…and also conducting virtual orientations for them through online platforms,” said Dr. Akre.
“If facilities face stockouts of contraception, women and girls will not be able to get the method of their choice,” she said.
*Name changed to protect privacy.